Ulcers: Types, Causes, Symptoms, Prevention, and Treatment
Table of Contents
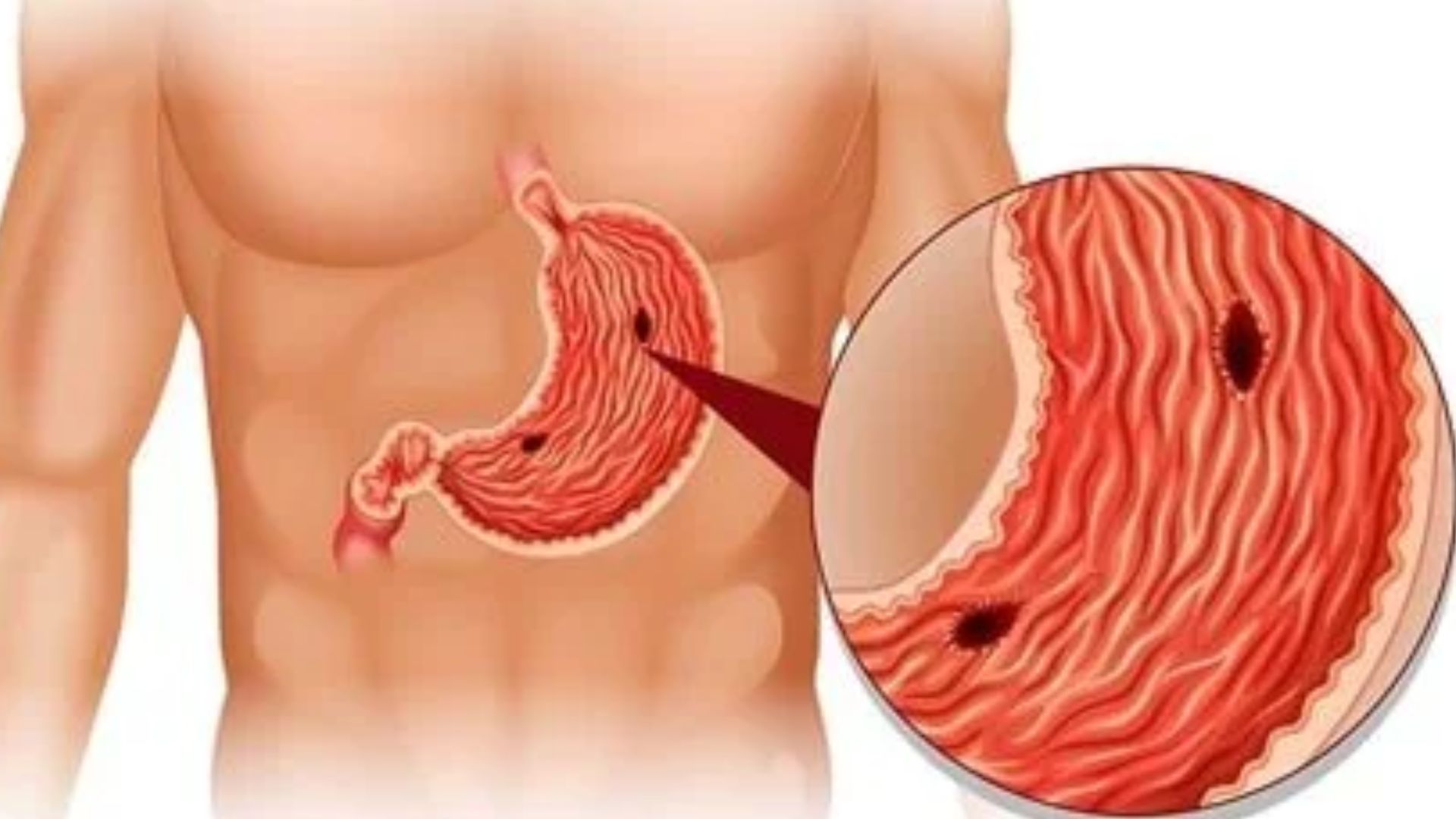
Ulcers are open sores or lesions that can develop on various parts of the body. While they can occur anywhere, they are most commonly found in the lining of the stomach, the small intestine, and the esophagus.
This article provides a comprehensive overview of ulcers, detailing the different types, their causes, symptoms, prevention strategies, and treatment options.
Types of Ulcers
There are several types of ulcers, each affecting different parts of the body:
1. Peptic Ulcers
Peptic ulcers are open sores that develop on the inner lining of the stomach and the upper portion of the small intestine. They are divided into two main types:
- Gastric Ulcers: These ulcers form on the lining of the stomach.
- Duodenal Ulcers: These ulcers occur on the lining of the duodenum, which is the first part of the small intestine.
2. Esophageal Ulcers
Esophageal ulcers are sores that develop in the lining of the esophagus, the tube that carries food from the mouth to the stomach. They are often associated with gastroesophageal reflux disease (GERD).
3. Mouth Ulcers
Mouth ulcers, also known as canker sores, are small, painful lesions that develop inside the mouth, on the gums, tongue, inner cheeks, or the roof of the mouth. They are usually harmless and resolve on their own.
4. Genital Ulcers
Genital ulcers are sores that appear on the genital organs. They can be caused by sexually transmitted infections (STIs), such as herpes simplex virus (HSV) and syphilis, or other non-infectious conditions.
5. Skin Ulcers
Skin ulcers are open sores that can occur anywhere on the skin. They are often the result of poor circulation, pressure, or injury, and can be associated with conditions such as diabetes and peripheral artery disease.
Causes of Ulcers
The causes of ulcers vary depending on their location and type. Here are the primary causes for each type:
Peptic Ulcers
- Helicobacter pylori (H. pylori) Infection: This bacterium is the most common cause of peptic ulcers. It damages the protective lining of the stomach and duodenum, allowing stomach acid to create an ulcer.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Regular use of NSAIDs, such as aspirin, ibuprofen, and naproxen, can irritate or inflame the lining of the stomach and small intestine, leading to ulcers.
- Excessive Alcohol Consumption: Drinking too much alcohol can damage the stomach lining and increase the production of stomach acid.
- Smoking: Smoking can interfere with the protective lining of the stomach and delay healing of existing ulcers.
- Stress: While stress alone does not cause ulcers, it can exacerbate existing ones by increasing stomach acid production.
Esophageal Ulcers
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux from the stomach into the esophagus can erode the lining and cause ulcers.
- Medications: Certain medications, such as bisphosphonates (used to treat osteoporosis) and certain antibiotics, can cause irritation and ulceration in the esophagus.
- Infections: Infections, particularly in immunocompromised individuals, can lead to esophageal ulcers.
Mouth Ulcers
- Injury: Biting the inside of the cheek, irritation from braces or ill-fitting dentures, and accidental burns from hot food can cause mouth ulcers.
- Nutritional Deficiencies: Deficiencies in vitamins such as B12, folate, and iron can contribute to the development of mouth ulcers.
- Stress and Hormonal Changes: These can trigger mouth ulcers in some individuals.
- Infections: Viral infections like herpes simplex can cause mouth ulcers.
Genital Ulcers
- Sexually Transmitted Infections (STIs): Infections like herpes simplex virus (HSV), syphilis, and chancroid are common causes of genital ulcers.
- Non-Infectious Conditions: Autoimmune diseases, such as Behçet’s disease, can also cause genital ulcers.
Skin Ulcers
- Poor Circulation: Conditions like peripheral artery disease and chronic venous insufficiency can lead to skin ulcers.
- Pressure: Prolonged pressure on the skin, especially in bedridden individuals, can cause pressure ulcers (bedsores).
- Diabetes: Poorly controlled diabetes can lead to diabetic ulcers, particularly on the feet.
Symptoms
The symptoms of ulcers can vary depending on their location and severity. Here are the common symptoms associated with each type:
Peptic Ulcers
- Burning Stomach Pain: A burning sensation in the stomach, often felt between meals or at night, is a common symptom.
- Bloating and Belching: These symptoms are often associated with peptic ulcers.
- Nausea and Vomiting: Some individuals may experience nausea and vomiting.
- Weight Loss: Unintentional weight loss can occur in severe cases.
- Dark, Tarry Stools: This can indicate bleeding in the stomach or duodenum.
Esophageal Ulcers
- Pain or Discomfort When Swallowing: This is a common symptom of esophageal ulcers.
- Chest Pain: Pain behind the breastbone, which can be mistaken for heart pain.
- Heartburn: A burning sensation in the chest or throat.
- Nausea and Vomiting: These symptoms can also be present.
Mouth Ulcers
- Painful Sores: Small, round, white or yellow sores with a red border inside the mouth.
- Difficulty Eating or Drinking: The pain can make eating and drinking uncomfortable.
- Swelling: Mild swelling around the ulcer.
Genital Ulcers
- Painful Sores: Open sores or lesions on the genital organs.
- Itching and Burning: These sensations are common around the sores.
- Swelling and Redness: Inflammation around the ulcers.
Skin Ulcers
- Open Sores: Open wounds that may ooze fluid or pus.
- Pain and Tenderness: The area around the ulcer is often painful and tender.
- Swelling and Redness: Inflammation around the ulcer.
- Delayed Healing: Skin ulcers often heal slowly and may recur.
How to Prevent Ulcer
Preventing ulcers involves addressing the underlying causes and risk factors. Here are strategies for preventing different types of ulcers:
Peptic Ulcers
- H. pylori Management: If you have an H. pylori infection, follow your healthcare provider’s treatment plan to eradicate the bacterium.
- Limit NSAIDs Use: Use NSAIDs sparingly and under the guidance of a healthcare provider. Consider alternative pain relief methods.
- Avoid Alcohol and Smoking: Reducing or eliminating alcohol consumption and quitting smoking can lower the risk of peptic ulcers.
- Stress Management: Practice stress-reducing techniques such as exercise, meditation, and relaxation exercises.
Esophageal Ulcers
- Manage GERD: Follow a treatment plan for GERD, which may include medications and lifestyle changes to reduce acid reflux.
- Medication Precautions: Take medications as prescribed and avoid those that can irritate the esophagus unless necessary.
- Avoid Irritants: Avoid foods and drinks that can exacerbate acid reflux, such as spicy foods, citrus fruits, and caffeine.
Mouth Ulcers
- Maintain Oral Hygiene: Brush and floss regularly to keep the mouth clean and reduce the risk of injury.
- Avoid Mouth Trauma: Be cautious when eating and avoid biting the inside of your mouth.
- Nutritional Supplements: Ensure you are getting adequate vitamins and minerals through diet or supplements.
Genital Ulcers
- Safe Sex Practices: Use condoms and have open discussions with partners about sexual health to reduce the risk of STIs.
- Regular Health Checkups: Regular screenings for STIs can help detect and treat infections early.
Skin Ulcers
- Maintain Good Circulation: Manage underlying conditions like diabetes and peripheral artery disease to promote good circulation.
- Pressure Relief: Change positions frequently if bedridden to prevent pressure on the area. Use specialized mattresses or cushions.
- Skin Care: Keep the skin clean and moisturized to prevent breakdown.

Treatment of Ulcers
The treatment of ulcers depends on their type and underlying cause. Here are the treatment options for different types:
Peptic Ulcers
Medications:
- Antibiotics: If H. pylori infection is present, a combination of antibiotics is used to eradicate the bacterium.
- Proton Pump Inhibitors (PPIs): These medications reduce stomach acid production and promote healing.
- H2-Receptor Antagonists: These drugs also reduce acid production and help heal ulcers.
- Antacids: Over-the-counter antacids can provide temporary relief from pain.
Lifestyle Changes:
- Dietary Modifications: Avoiding spicy and acidic foods can help manage symptoms.
- Stress Management: Techniques such as meditation, yoga, and exercise can reduce stress, which may exacerbate ulcer symptoms.
- Smoking Cessation: Quitting smoking can improve the healing of wounds and reduce the risk of recurrence.
- Limit Alcohol: Reducing alcohol consumption can prevent irritation of the stomach lining.
Surgery:
In rare cases, surgery may be necessary if an ulcer does not heal with medication or if complications such as bleeding, perforation, or obstruction arise. Surgical options include:
- Vagotomy: Cutting the vagus nerve to reduce acid secretion.
- Antrectomy: Removing the lower part of the stomach that produces gastrin, a hormone that stimulates acid production.
- Pyloroplasty: Widening the opening of the pylorus (the lower part of the stomach) to allow contents to pass more easily into the duodenum.
Esophageal Ulcers
Medications:
- PPIs and H2-Receptor Antagonists: These medications reduce acid production and promote healing.
- Antibiotics: If an infection is present, antibiotics may be prescribed.
Lifestyle Changes:
- Elevating the Head of the Bed: Sleeping with the head of the bed elevated can reduce nighttime reflux.
- Eating Smaller, More Frequent Meals: This can prevent the stomach from becoming too full and reduce reflux.
- Avoiding Trigger Foods and Beverages: Spicy foods, citrus, chocolate, caffeine, and alcohol can exacerbate symptoms and should be avoided.
- Weight Management: Maintaining a healthy weight can reduce pressure on the stomach and esophagus.
Mouth Ulcers
Medications:
- Topical Treatments: Gels, creams, and mouth rinses containing corticosteroids, antiseptics, or analgesics can reduce pain and inflammation.
- Oral Medications: In severe cases, oral corticosteroids or other medications may be prescribed.
Home Remedies and Lifestyle Changes:
- Good Oral Hygiene: Brushing with a soft-bristled toothbrush and using an alcohol-free mouthwash can prevent irritation.
- Avoiding Irritants: Steering clear of spicy, acidic, or rough-textured foods can prevent further irritation.
- Nutritional Supplements: Taking vitamins and minerals if deficiencies are identified can help prevent recurrence.
Genital Ulcers
Medications:
- Antiviral Drugs: For herpes simplex virus (HSV) infections, antiviral medications such as acyclovir, valacyclovir, and famciclovir can reduce symptoms and prevent outbreaks.
- Antibiotics: For bacterial infections like syphilis or chancroid, appropriate antibiotics are prescribed.
- Pain Relief: Over-the-counter pain relievers and topical anesthetics can alleviate discomfort.
Lifestyle and Preventative Measures:
- Safe Sex Practices: Using condoms and having open discussions with partners about sexual health can reduce the risk of sexually transmitted infections.
- Regular Medical Checkups: Routine screenings for STIs and other health conditions can help detect and treat issues early.
Skin Ulcers
Medications:
- Topical Antibiotics: For infected ulcers, topical antibiotics can help clear the infection.
- Oral Antibiotics: Severe or widespread infections may require oral antibiotics.
Wound Care:
- Cleaning and Dressing: Keeping the wound clean and covered with appropriate dressings can promote healing and prevent infection.
- Debridement: Removing dead or damaged tissue from the ulcer site to promote healing.
Lifestyle Changes:
- Pressure Relief: Regularly changing positions and using cushions or specialized mattresses can prevent pressure ulcers.
- Good Nutrition: A balanced diet rich in vitamins and minerals supports skin health and healing.
- Blood Sugar Management: For diabetics, keeping blood sugar levels under control can prevent diabetic ulcers.
Conclusion
Ulcers are a diverse group of conditions that can affect various parts of the body, each with its own causes, symptoms, prevention strategies, and treatment options. Understanding these aspects is crucial for effective management and prevention of complications.
Whether peptic, esophageal, mouth, genital, or skin ulcers, recognizing the signs and seeking appropriate medical advice is essential for optimal care and recovery.
Continue reading: Types of Cancer: The different stages and grades